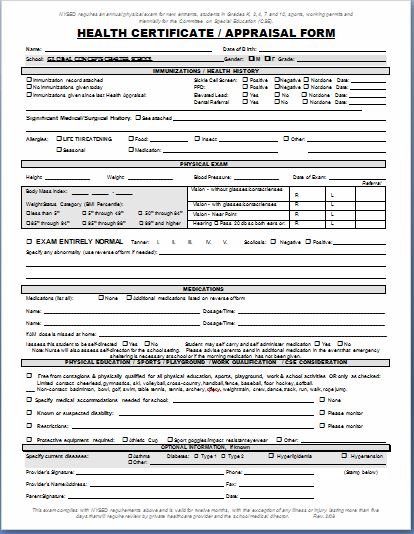
Sample Written History and Physical ExaminationHistory and Physical Examination CommentsPatient Name: Rogers, PamelaDate: 6204Referral Source: Emergency DepartmentData Source: PatientChief Complaint ID: Ms. Rogers is a 56 yo WF Define the reason for the patients visit as who has beenhaving chest pains for the last week. Sample Written History and Physical Examination History and Physical Examination Comments Patient Name: Rogers, Pamela Date: 6204 Referral Source: Emergency Department All View Text Version Report. Related publications Sample Written History and Physical Examination. Sample Written History and Physical Examination History and Physical. Sample WriteUps Sample Neurological HP CC: The patient is a 50yearold righthanded woman with a history of chronic headaches who complains of acute onset. The purpose of the questions in this form is to gather information concerning your health and physical condition, both now and in the past. 02 requires that officers be found, after examination by a licensed physician or surgeon, to be free from any physical, emotional, or mental conditions which might adversely affect hisher exercising the powers or duties of a peace officer. 25 Medical Report Samples In order for medical professionals to know a patients progress or medical status, creating medical reports are what they need. A medical report is an updated detail of a medical examination of a certain patient. The history and Mental Status Examination (MSE) are the most important diagnostic tools a psychiatrist has to obtain information to make an accurate diagnosis. Causes Multiple etiologies based on findings from history, MSE, physical examination, lab studies, and other required diagnostic tests. Example of a Complete History and Physical Writeup Patient Name: Unit No: Location: Informant: patient, who is reliable, and old CPMC chart. Chief Complaint: This is the 3rd CPMC admission for this 83 year old woman with a long history of hypertension who presented with the chief complaint of substernal toothache like chest pain of 12 hours A physical report is a type of report that is given after a physical examination has taken place and is often times used as a way to determine a persons physical capabilities and whether they are able to physically handle the task assigned to them. Sample Written History and Physical Examination History and Physical Examination Comments Patient Name: Rogers, Pamela Date: 6204 Referral Source: Emergency Department Data Source: Patient Chief Complaint ID: Ms. Rogers is a 56 yo WF Define the reason for the patients visit as who has been having chest pains for the last week. A complete history and physical examination can identify important health issues that may be solved at the domestic medical examination visit or more chronic conditions that need further evaluation or. The above analysis is based upon the available information at this time, including the history given by the examinee, the medical records and tests provided, the results of pain status inventories, and the physical findings. PHYSICAL EXAMINATION: Weight is 202 lb consultation family history History and Physical medical transcription samples mt samples past medical history past surgical consultation family history History and Physical medical transcription samples mt samples past medical history past surgical. Page 1 SAMPLE HISTORY and PHYSICAL History and Physical Examination of P. Performed in Emergency Department, 2: 00PM History and Physical Examination A 46yearold female was referred for an EDX examination because of increasing problems with numbness in tingling in her left hand over the last 3 years. 8 The psychiatric history and mental state examination (MSE) The psychiatric history and mental state examination (MSE) In taking a psychiatric history and assessing the mental state, it is Informant history Physical examination KRP01 5: 27 PM Page 8. What the candidate reads Candidates instructions. Lynne Black, 20 years old, presents to the Emergency Department with a 16hour history of abdominal pain. In the next 10 minutes, obtain a focused and relevant history and conduct a focused and relevant physical examination. MEDICAL TRANSCRIPTION SAMPLE REPORT HISTORY AND PHYSICAL EXAMINATION DATE OF ADMISSION: ADMITTING PHYSICIAN: CHIEF COMPLAINT: I passed out. MEDICAL TRANSCRIPTION SAMPLE REPORT HISTORY AND PH Today's scenario there are many persons like hous My Blog List. despite strong evidence from the history and physical examination. This will result in a lower score. History can be presented in The examinee has described the findings relevant to the back pain, and is not required to report a complete physical examination. Medical Examination Report Form (for Commercial Driver Medical Certification) Comment on the driver's responses to the health history questions that may affect the driver's safe operation of a commercial motor vehicle (CMV). The Physical Examination (PE) is an objective assessment of the patients condition. The examiner observes, pokes, and prods the patient and records the results here. In some report types, a brief, focused exam may be conducted, but an exam done as part of an HP typically assesses the patient from head to toe, one body system at a time. Medical History and Physical Examination. testing required to determine the aliens status regarding Class A and Class B conditions and to complete the medical report form. If the examination reveals an acute illness that makes it impossible to determine the aliens medical status regarding Class A or B. A physical examination, medical examination, or clinical examination (more popularly known as a checkup) is the process by which a medical professional investigates the body of. view is a brief history and physical examination specically reviewing the cardiopulmonary, integumentary, musculoskeletal, and neuromus cular systems, but. The following history does not correspond to any specific case or diagnosis. This is the first admission for this 56 year old woman, who states she was in her usual state of good health until one Written History and Physical Examination History and Physical Sample Report (General) 8: 33 PM blog it No comments HISTORY OF PRESENT ILLNESS: This is a 43yearold black man with no apparent past medical history who presented to the emergency room with the chief complaint of weakness, malaise and dyspnea on exertion for approximately one month. Rehabilitation Medical Transcription History and Physical Sample Report DATE OF ADMISSION: MMDDYYYY HISTORY OF PRESENT ILLNESS: This is a (XX)yearold male admitted to (XX) Hospital, MMDDYYYY, after falling in the bathtub and found to be unresponsive. History and Physical Examination (HP) Examples; Educational Activities; Accommodations Information for OSCENBME Exam; History and Physical Examination (HP) Examples Info. The links below are to actual HPs written by UNC students during their inpatient clerkship rotations. The students have granted permission to have these HPs posted on the. The HEENT, or Head, Eye, Ear, Nose and Throat Exam is usually the initial part of a general physical exam, after the vital signs. Like other parts of the physical exam, it begins with inspection, and then proceeds to palpation. History and Physical Examination, the introduction, preparation, history, examination, and more about History and Physical Examination. History and Physical Examination, the introduction, preparation, history, examination, and more about History and Physical Examination. if you would like to report a specific issue. History and Physical (H and P) Medical Transcription Sample Reports for Medical Transcriptionists This page has moved and can be found at the updated address below. Click on link below to access it. An Example of a History, Physical Examination, Presentation and Problem Solving Practical Examination Station (Department of Internal Medicine, The University of Texas Medical Branch) History and Physical Medical Transcription Sample Report# 2 DATE OF ADMISSION: MMDDYYYY HISTORY OF PRESENT ILLNESS: The patient is a (XX)yearold Hispanic female with history of severe hypertension, diabetes mellitus, cerebrovascular disease, status post CVA x4. A physical exam form is a blank form and format with guided lines that tells you what to fill up on each blank space, and gives you this ready format to make a complete report of the physical examination of a candidate who is ready to apply for something, go somwhere or getting ready for some special work or. Physical Examination and History Taking CHAPTER 1 Overview of Physical Examination and History Taking the health history, the physical examination, and the written record, or write report may be needed. Varies according to the patients memory, trust, and mood. 7 Sample Physical Report Forms Health is wealth, as an old adage says, which is why having periodic Physical Exams are necessary. A Physical Exam is a way of conducting preventive treatment for everyone regardless of race, age, sex, or level of activity. [0046c3 Sample History And Physical Examination Report sample written history and physical examination history and physical examination comments patient name rogers pamela date 6 2 04 referral Taking the patient's history is traditionally the first step in virtually every clinical encounter. A thorough neurologic history allows the clinician to define the patient's problem and, along with the result of physical examination, assists in formulating an. The gynecologic history and physical examination in adult women are reviewed here. The initial assessment of pregnant women, evaluation of breast complaints, general approaches to patient interviewing as well as pelvic examination in children are discussed separately. History and Physical notes transcription services with price tag not exceeding a third of local US service rates the physician is required to dictate a History and Physical Report patient medical history, present medications, family medical history, surgery history, physical scrutiny. Clinic History and Physical MedicalTemplate Read online for free. The clinic history and physical (Clinic HP) MedicalTemplate is suitable for internal medicine physicians, family practice physicians, and other health care providers that evaluate patients in clinics or other outpatient settings. Write Ups The written History and Physical (HP) serves several purposes: It is an important reference document that gives concise information about a patient's. The examination is, in general, a report by test, wherein each test applied during the examination is stated and the results are reported, whether the results are favorable or unfavorable. Watch Queue Queue Taking a history is the initial step in the physicianpatient encounter. This provides a basis for emphasizing aspects of the subsequent physical examination, and for initial decisions about diagnostic testing and treatment. GYN History and Physical Chief Complaint: HPI First sentence should include age, parity, LMP and present problem (details about cc and other relevant information). DATA BASE SAMPLE: PHYSICAL EXAMINATION WITH ALL NORMAL FINDINGS GENERAL APPEARANCE: (include general mental status) 45 yo female who is awake and alert and who appears healthy and looks her stated age VITALS Temperature: 37. 5 C oral (list the site where the temperature was taken, i. 1 THE HISTORY AND PHYSICAL (H P) I. Chief Complaint according to Bates' A Guide to Physical Examination, the present illness. should include the onset of the problem, discoloration of lips or nailbeds (cyanosis), history of exposure to TB, history of a previous TB skin test and the results if done, recurrent pneumonia, history. : Patient is gravada 2, para 1, abortus 1. The patients only child is a 15 year old daughter who lives in Texas with her grandmother. PAST MEDICAL HISTORY: Patient had a Pilonidal cyst removed. SAMPLE history is an mnemonic acronym to remember key questions for a person's medical assessment. The SAMPLE history is sometimes used in conjunction with vital.









.jpg)